Affordable Group Health Insurance Plans
Keep your team happy, healthy, and engaged. We'll guide you to the right health insurance plan while navigating compliance and staying within your budget.
Get the health coverage your team deserves:
|
|
Enroll your employees seamlessly |
|
|
Choose from multiple top-tier plan providers |
|
|
Integrate effortlessly with your payroll |

Benefits of Paychex Group Health Plans
Integrated Benefits and Payroll
Connect your group health plan to your payroll system to:
- Minimize data entry errors
- Reduce administrative costs
- Save time with smooth, automated data transfers between systems

Easy Enrollment in One Place
Our integrated platform lets you:
- Give employees real-time access to benefits through a mobile app
- Streamline enrollment, carrier updates, and payroll
- Enhance benefits communication with tips and alerts

Fulfill Affordable Care Act (ACA) Requirements
Our group health insurance solutions help you navigate ACA compliance by:
- Assessing coverage to meet reporting requirements
- Managing form submissions with accuracy and efficiency
- Offering expert support to stay informed on rule changes and help maintain compliance

Licensed Agents Can Help
Licensed agents are available to help you choose the right group health plan for your employees and coordinate with carriers.

Enhance Your Health Benefits With Extended Plans and Services
What You Can Expect With Paychex Group Health Insurance
Partner with Experts for Tailored Solutions
Our licensed agents streamline benefits for your business. We’ll compare plans based on your needs and budget, gathering quotes from top carriers and helping you find the perfect fit.
Seamless Employee Enrollment
Let our team guide your employees through the enrollment process- no confusion, no stress.
Hassle-Free Package Submission
Once ready, we’ll submit your package to the carrier for underwriting and rates, ensuring accuracy to avoid delays and get everyone covered quickly.
Unmatched Client Support
Our Client Service Specialists are available anytime to assist with claims, coverage issues, or carrier coordination. We’re here to support your success every step of the way.
All-in-One HR & Payroll with Benefits That Work for You
Get exactly what you need — nothing you don’t. Easily integrate with your existing payroll provider or upgrade with Paychex payroll and HR plans.
Explore our packages today!

Seamless Solutions for Managing Benefits
Stay on top of managing eligibility tracking, enrollment forms, benefit changes, and more with our automated benefits platform.
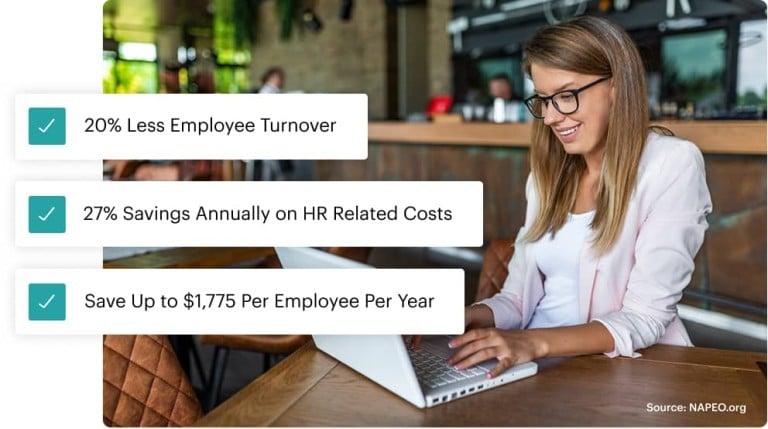
Reimagine Benefits with PEO Support
A PEO (Professional Employer Organization) is like having an HR partner. We handle payroll, benefits, and compliance while you get enterprise-level benefits for your team and more time to focus on your business.
Get More Value from Your Benefits Platform
Experience integrated solutions that work together in one easy-to-use platform.
Recommended for You
Group Health Insurance FAQs
-
What Is a Group Health Plan?
What Is a Group Health Plan?
A group health insurance plan is a benefit offered by businesses or organizations to provide health coverage for employees or members. It helps attract top talent, retain employees, and offers potential tax savings.
-
What Are Examples of Group Health Plans?
What Are Examples of Group Health Plans?
Group health plans offer various options for employee health insurance coverage:
- Health Maintenance Organization (HMO): Requires a primary care physician (PCP) within a network and referrals for specialists, often with lower out-of-pocket costs.
- Preferred Provider Organization (PPO): Provides flexibility to see in-network and out-of-network providers, with lower costs for in-network care.
Other options include Exclusive Provider Organizations (EPO) and High-Deductible Health Plans (HDHP).
-
How Many Employees Do You Need to Qualify for Group Health Insurance?
How Many Employees Do You Need to Qualify for Group Health Insurance?
Group health insurance usually requires at least two people, including the owner, though specific rules can vary depending on your state and insurance carrier. PEOs require 5 employees with minimum group participation requirements. Be sure to check with your provider for exact requirements. If you don’t qualify for group coverage, individual health plans may be a good alternative to explore.
-
What Is Included in A Comprehensive Employee Benefits Package?
What Is Included in A Comprehensive Employee Benefits Package?
A group health insurance plan covers specific medical expenses for you and your participating employees. Group dental, vision plans, and other voluntary insurance are offered separately.
-
How Do Group Insurance Policies Work?
How Do Group Insurance Policies Work?
Group health plans let employers offer comprehensive health coverage to employees at lower costs than individual health plans. By leveraging group buying power, employers negotiate better rates, with premiums typically shared between the employer and employees. These plans are often more affordable than individual marketplace options.
-
What Is the Difference Between Group Insurance and Individual Plans?
What Is the Difference Between Group Insurance and Individual Plans?
Group insurance covers two or more people, such as employers, employees, and their families. Individual insurance covers one person, with options to add eligible family members. For sole proprietors or freelancers, individual insurance offers essential coverage when group plans aren't available. It also allows employees to customize their coverage and choose their own provider instead of relying on employer-selected plans.
-
How Do I Choose the Right Group Health Insurance for Employees?
How Do I Choose the Right Group Health Insurance for Employees?
Choosing group health insurance requires balancing cost and value. While it’s a major expense, offering quality benefits helps attract and retain top talent. Compare multiple carriers and plans, focusing on:
- Coverage and affordability balance
- Co-pay, prescription, and hospitalization options (note: more coverage means higher premiums)
-
How To Choose Group Health Insurance for My Small Business?
How To Choose Group Health Insurance for My Small Business?
Choose group health insurance by evaluating your budget, employee needs, and comparing provider plans. Aim for affordable coverage with strong benefits to support your team.



